Check out the latest issue of the AFT publication Health Care which includes an article by our very own Donna Phillips and Stacey Sever titled “Standing Up For Alaska’s Nurses”
Article below is from AFT Health Care, Spring 2024 found at: https://www.aft.org/hc/spring2024/phillips_sever
Standing Up for Alaska’s Nurses
By Donna Phillips, Stacey Sever
In Alaska, our staffing and retention problems can be exacerbated by the remoteness of our facilities. For example, we have only one long-term acute care hospital in Alaska—and in Providence Alaska Medical Center alone, we have dozens of patients who don’t meet inpatient or skilled nursing home criteria but have nowhere else to go. Administration said they wanted to put those long-term patients on one wing of the med-surg floor with a nine-to-one patient-to-nurse ratio. Naturally, our nurses revolted. Union members went to town halls to speak their minds and wore bright red badges in protest. Within two weeks, the hospital backed down, and they haven’t revisited it since.
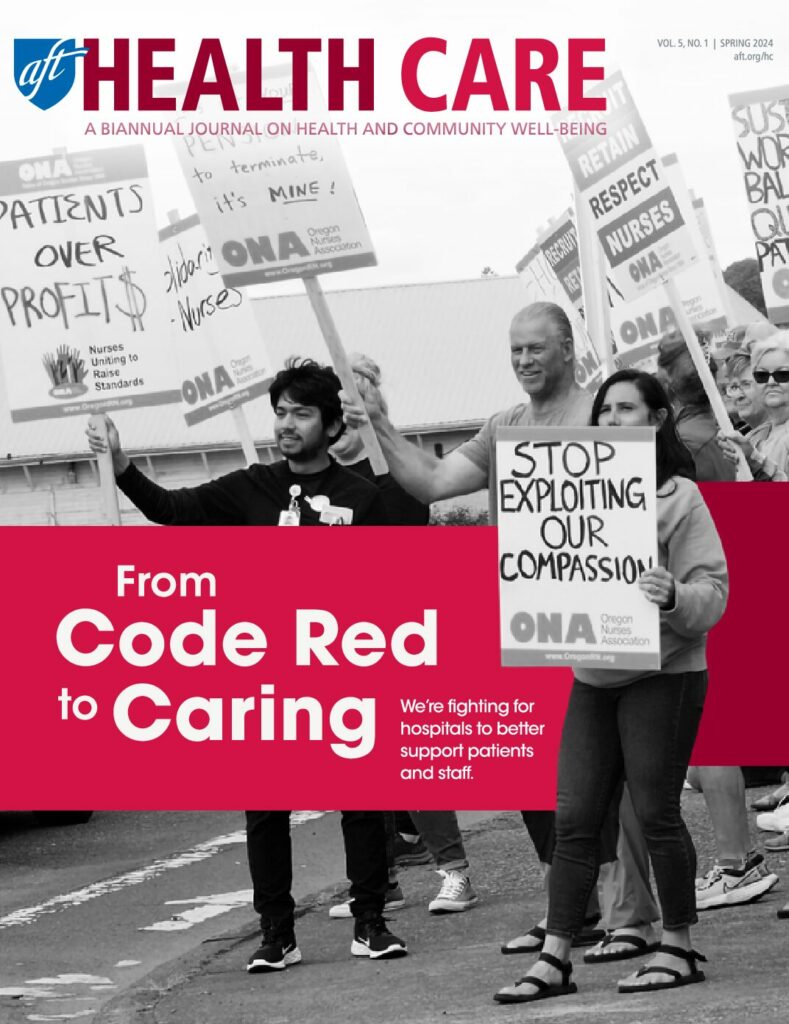
We’re continuing to use our power to check hospitals’ greed, including by incorporating staffing ratios into our contract campaigns—but we don’t expect that healthcare employers in Alaska are going to commit to safe staffing ratios without legislation. Our staffing committees function more like scheduling committees, and employers like Providence try to change staffing plans at will. That’s why staffing legislation is the primary focus of our Code Red campaign.
We’re preparing for a long campaign, starting with research. We are working with AFT staff to develop a white paper on the need for safe staffing ratios in Alaska hospitals, and we’re asking our nurses to complete a brief staffing survey so we have data on current workplace conditions. We plan to use both as foundations of our campaign as we hold lobby days and lay the groundwork for legislation.
We also know that there’s more we can do to help Alaska nurses sooner.
One major staffing issue has to do with preparation. There’s a shortage of instructors because nurses with five years’ experience can make more at the bedside than a nurse with a PhD does teaching. Students who get coveted spots in nursing programs graduate with thousands of dollars of debt; some facilities give a sign-on bonus or other incentives, but if nurses leave before a specified time, they often have to return part of that bonus. Unfortunately, there’s no way to know in advance that the job will be a good fit or that new nurses will get the support they need.
We have programs that attempt to address some of these issues, but sometimes they create additional problems. For example, the residency program at Providence Alaska Medical Center brings in three cohorts of about 40 recently graduated RNs each. The staff nurses do their best to train the new nurses, but they don’t get a lesser assignment so that they have time for the work of precepting. We’re also finding that because of short staffing, these new nurses are asked to start taking assignments before they’ve completed their residency.
If the facilities that desperately need the next generation of nurses took on more financial responsibility for preparing them, that would be a huge help. There’s pressure to change licensure requirements and decrease the quality of care we provide because these facilities don’t have enough staff—but where are they when it comes to cultivating that staff?
We’re working with a legislator on a bill that would establish nurse apprenticeships so that students would get paid while they’re learning nursing hands-on from experienced nurses, much like the trades do. Apprentices would gain experience as they help turn and walk patients and do other time-consuming tasks RNs are asked to do, and they would benefit from spending a lot more time in the hospital before graduation. You can read about what happens when someone goes into pulmonary edema or has any change in condition that requires quick intervention—but seeing it is completely different. If you have that first experience before your residency or first job, you have a huge advantage (and so do your patients).
We’re also educating members and our community about the importance of the political process. If we want to pass legislation, we need to get people elected who will support it, from the governor down to the local level. We’re writing about it in Alaska Nurse and other publications and talking about it at our conferences. We also went door knocking to get out the vote for the mayoral and school board races in Anchorage. Nurses need to understand how important it is to know their elected officials and tell them what’s happening at work.
We’re committed to winning protections for Alaska healthcare workers and patients. We prefer collaborating with administrators, but we’re fighting to make the most of those opportunities.
Donna Phillips, BSN, RN, is the labor council chair of the Alaska Nurses Association and an AFT vice president; she was an intensive care unit nurse for 44 years, with 29 years advocating for union nurses and Alaskans at Providence Alaska Medical Center. Stacey Sever, BSN, RN, CCDS, is a former emergency room and flight nurse with Providence Health & Services and the health and safety committee chair of the Alaska Nurses Association.
AFT Health Care, Spring 2024